No, Hormone Replacement Therapy Does Not Increase Your Risk of Cancer
How a Flawed 2002 Study Misled a Generation of Women— and Why the FDA’s Removal of a Warning Label Matters
By Catherine Ebeling, RN, MSN, Contributor, The MAHA Report
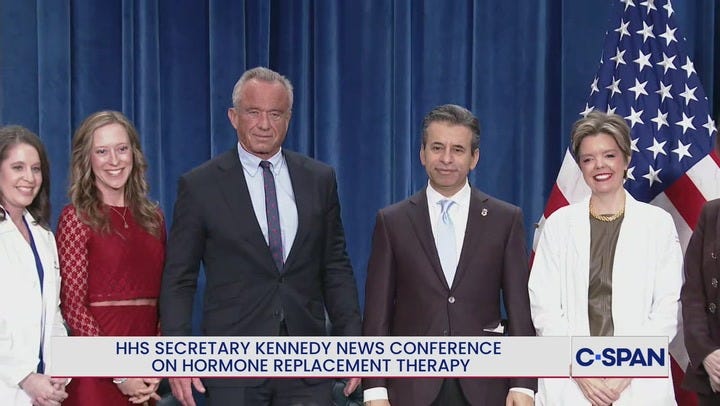
On Monday, November 11, Health and Human Services (HHS) Secretary Robert F. Kennedy Jr. announced that the black box warning on women’s estrogen products for hormone replacement therapy (HRT) will be removed, according to The Hill.
“For more than two decades, the American medical establishment turned its back on women,” Kennedy said at a press briefing at HHS headquarters. “Millions of women were told to fear the very therapy that could have given them strength, peace, and dignity through one of life’s most difficult transitions—menopause.”
Both Kennedy and Food and Drug Administration (FDA) Commissioner Marty Makary pointed to the flawed Women’s Health Initiative (WHI) study from more than 20 years ago that first suggested hormone replacement therapy could increase breast cancer risk.
“The Women’s Health Initiative study was the largest study ever done in U.S. history, [and]…that study was misrepresented and created a fear machine that lingers to this day,” Makary told The Hill. “There’s no statistical significance in the increase in breast cancer. If we don’t have statistics, then we don’t have science.”
The Way It Was
In 2002, women’s hormone health and overall health and wellbeing was drastically changed for the worse. The Women’s Health Initiative (WHI) released results claiming that HRT for premenopausal and menopausal women (most commonly ages 45 - 55) increased breast cancer, stroke, and heart disease risk. Within weeks, millions of women stopped taking estrogen, and doctors started preaching hormone fear to their female patients.
The HHS announcement earlier this week marks an historic turning point in women’s health—and a long-overdue correction to one of medicine’s most damaging missteps.
Two decades later, we now know that the WHI’s conclusions were based on a deeply flawed study and wildly over-generalized data. The result has been one of the most damaging public health misunderstandings and medical ‘myths’ in
modern medicine.
Why the WHI Study Was Flawed
The WHI was not a single study but actually two hormone-therapy trials under a massive NIH (National Institute of Health) umbrella project. It enrolled 27,347 women across a very broad age group – 50–79 year-olds. The problem was that the average age of participants was 63—a full decade older than the typical woman who starts hormone therapy at menopause. This study should have included women aged 45-55, not an older segment of the female population.
The interventions used in the study included:
Conjugated equine (horse) estrogen, or CEE 0.625 mg, Premarin, which is a synthetic estrogen.
Medroxyprogesterone acetate, or MPA 2.5 mg, Provera, a synthetic progestin in women with a uterus.
Or CEE alone in women who had had a hysterectomy.
The goal was not to study symptom relief (hot flashes, etc) or quality of life, but to test if hormones could prevent chronic conditions such as heart disease, dementia, and osteoporosis in older women who were post-menopause.
In other words, the WHI was asking the wrong question of the wrong population using the wrong drugs.
Flaw #1: The Wrong Population
As mentioned, most women who need hormone therapy are 45-55 years old, and within a few years of their final menstrual period. By contrast, the WHI participants were, on average, 12 or so years post-menopause.
At menopause, the risk for chronic diseases such as heart disease, osteoporosis, dementia, diabetes, and breast cancer goes up significantly. So, many of the women in the study who were post menopause, already had the beginnings of metabolic disease, heart disease, breast cancer, and other chronic diseases.
We now understand that starting oral estrogen late, after arterial plaque has formed, can temporarily increase risk of clotting or stroke risk. Later re-analysis of the WHI data confirmed the ‘timing hypothesis,’ which was that women who began hormones before age 60 or within 10 years of menopause, had lower cardiovascular mortality and total mortality than placebo users.
Flaw #2: The Wrong Drugs
The WHI didn’t use bioidentical hormones – hormones that are molecularly the same as the body’s natural hormones, and are utilized as natural hormones. The synthetic hormones used in the study were molecularly different from natural human estrogen and progesterone. This matters greatly.
More recent studies show that using bioidentical ‘transdermal’ (absorbed through skin) hormones, or ‘sublingual’ (absorbed through membranes in the mouth) hormones are absorbed directly into the bloodstream and not metabolized in the liver, lowering blood clotting risk.
Micronized bioidentical progesterone, unlike the synthetic version (progestin) used, shows neutral or protective effects on breast tissue and cardiovascular markers.
So what the WHI told us only that an outdated oral synthetic combination did not prevent chronic disease—not that ALL female hormones of all types, on all ages of women, were dangerous.
Flaw #3: The Wrong Question
The WHI study did not even try to answer what most women and clinicians wanted to know: “Is hormone therapy safe and effective for relieving menopausal symptoms and preserving long-term health if started near menopause age?”
Instead, it tested whether hormones could prevent chronic disease in women already well past menopause. As mentioned above, the problem is that the risk of chronic disease goes up significantly at menopause, so many of the women in the study already had the beginnings of chronic disease, due to their older age.
When, in 2002, data suggested a 26 % relative increase in breast-cancer risk in the combined synthetic estrogen and progestin, media headlines screamed “Women’s Hormones Cause Cancer.”
The actual numbers were less than 1 per 1000 per year, a very small absolute difference.
However, that same study showed fewer hip fractures, lower rates of osteoporosis, and lower incidence of colon cancers. The synthetic estrogen only arm of the study showed a reduced breast-cancer incidence and mortality. None of those important health factors actually made the news.
Flaw #4: Early Termination and Oversimplified “Global Risk”
The combined-therapy trial was stopped after only 5.2 years—way before the long-term benefits of hormone therapy could emerge. Researchers also used a “global index” that lumped together heart disease, stroke, breast cancer, and osteoporosis, but ignored vital quality-of-life measures like better sleep, improved mood, increased libido, and better cognitive health—all important issues that matter enormously to women.
Stopping the study early inflated apparent risks and distorted the risk-benefit balance.
Flaw #5: Real-World Damage to Women
The WHI headlines triggered a 70 % drop in hormone prescriptions almost overnight. Menopause research funding dried up. Thousands and thousands of women suffered from untreated hot flashes, insomnia, depression, anxiety, low libido, bone loss, heart disease, and cognitive decline—all life-changing health issues that could have been managed with proper treatment.
But 23 years later, the recent HHS announcement is already inspiring some women. “Today’s decision restores balance to women’s health policy. For years, risk was overstated and benefit was understated,” Monique Yohanan, senior fellow for health policy at the conservative nonprofit Independent Women, told The Hill earlier this week. “Today, fewer than 5 percent of post-menopausal U.S. women use menopausal hormone therapy, down from 25-30 percent two decades ago.”
What We Know Now
More up-to-date hormone therapy now recommends transdermal or sublingual delivery. While many women report better effects with bioidentical hormone replacement therapy, more research is needed on synthetic vs. bioidentical hormone replacement safety and efficacy.
However, for healthy women within ten years of menopause, the benefits of hormone replacement outweigh the risks.
Why This Matters
The WHI story is not just about hormone replacement. It’s a cautionary tale about how science is often misinterpreted, weaponized by fear, and cemented into policy. Sound familiar?
It exposed the blind spot in our public health system: how one over-simplified narrative can derail decades of women’s health. This is much like the many ‘health myths’ that are perpetuated by the mainstream medical system, and Big Pharma, that have tied flawed studies and faulty research to misaligned diagnoses and treatment.
Hormone therapy, especially bioidentical hormone therapy, started at the right time, with the best delivery method, can drastically improve quality of life, protect bone, heart, and brain health, and reduce all-cause mortality.
It’s time to set the record straight – and that’s the beauty of what HHS Secretary Kennedy and FDA Commissioner Makary did this week.





I remember clearly this debacle and the overnight fear that enveloped my patients on HRT.. I had a hard time even then accepting that study because with my small brain and basic " country doc knowledge " I could see the flaws.. I cautioned my patients and let them choose based on risk/ benefit. Never saw any rise in the touted side effects listed in this wretched study.. Clinical experience and anecdotal evidence speaks for itself.. sadly a whole generation has lost this benefit and current physicians are still behind in knowledge. Most patients are way more educated on this topic than their PCP/GYN!!
Edited to add: one key point is now I am a little worried the pendulum may shift too far the other way, almost akin to the days of " nursing shaming " . Social media influencers and famed gynecologists on social media are now preaching HRT benefits from the rooftops and extrapolating almost guaranteed health benefits in multiple health dark horses .. the fact is HRT has been studied less in women than the animal/ good industry and now as being sold as the new wonder drug for all. It's definitely not the answer for everyone and many choose not to use it or have genetic issues and conditions that make it intolerable. More studies are needed but caution needs to be heeded so we don't make false promises or misinform or shame those for whom HRT causes more issues than helps.
Medicare and my supplemental won't cover bioidentical only synthetic hormones, hopefully this will change.